In silico targeting enterotoxin from Staphylococcus aureus with selected flavonoids: Hope for the discovery of natural anti-mastitis agents
DOI:
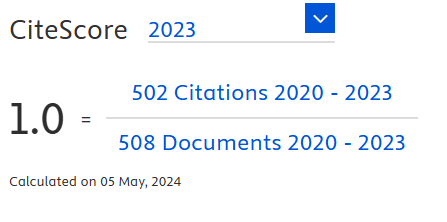
https://doi.org/10.18006/2023.11(1).132.139Keywords:
Enterotoxin, S. aureus, Phytochemicals, Mastitis, Molecular dockingAbstract
Staphylococcus aureus is a facultative anaerobe and catalase-positive bacterium responsible for various skin infections and life-threatening problems, including bacteremia and pneumonia. This bacterium produces a bunch of superantigens in the blood called enterotoxin. This toxin is responsible for food poisoning and toxic shock syndrome. Moreover, Bovine mastitis is also associated with S. aureus. Further, S. aureus related to drug resistance makes the infection more dreadful. Now a day, various natural compounds such as phytochemicals are gaining importance as they are effective against many diseases, including S. aureus infections. The present study used molecular docking of three ligands, i.e., Kaempferol, Apigenin, and Quercetin, with enterotoxin A from S. aureus. The docking study revealed that the binding energy of ligands with receptors was -6.6 to -6.9 Kcal/mol. Kaempferol had the highest binding affinity of -6.9 Kcal/mol, suggesting it has a potential against S. aureus. Therefore, in the current research, we have tried to identify occurring compounds that might be used to develop an effective anti-S.aureus agent. The findings are encouraging and will aid researchers in creating new mastitis-fighting medications based on natural phytochemicals.
References
Ahmad-Mansour, N., Loubet, P., Pouget, C., Dunyach-Remy, C., Sotto, A., Lavigne, J. P., & Molle, V. (2021). Staphylococcus aureus Toxins: An Update on Their Pathogenic Properties and Potential Treatments. Toxins, 13(10), 677. https://doi.org/10.3390/TOXINS13100677 DOI: https://doi.org/10.3390/toxins13100677
Bansal, P., Tuli, H. S., Sharma, V., Mohapatra, R. K., Dhama, K., Priti, & Sharma, A. K. (2022). Targeting Omicron (B.1.1.529) SARS CoV-2 spike protein with selected phytochemicals: an in-silico approach for identification of potential drug. Journal of Experimental Biology and Agricultural Sciences, 10(2), 396–404. https://doi.org/10.18006/2022.10(2).396.404 DOI: https://doi.org/10.18006/2022.10(2).396.404
Cassat, J. E., & Thomsen, I. (2021). Staphylococcus aureus infections in children. Current Opinion in Infectious Diseases, 34(5), 510–518. https://doi.org/10.1097/QCO.0000000000000752 DOI: https://doi.org/10.1097/QCO.0000000000000752
Chakraborty, S., Dhama, K., Tiwari, R., Iqbal Yatoo, M., Khurana, S. K., Khandia, R., Munjal, A., Munuswamy, P., Kumar, M. A., Singh, M., Singh, R., Gupta, V. K., & Chaicumpa, W. (2019). Technological interventions and advances in the diagnosis of intramammary infections in animals with emphasis on bovine population-a review. The Veterinary Quarterly, 39(1), 76–94. https://doi.org/10.1080/01652176.2019.1642546 DOI: https://doi.org/10.1080/01652176.2019.1642546
Cheung, G. Y. C., Bae, J. S., & Otto, M. (2021). Pathogenicity and virulence of Staphylococcus aureus. Virulence, 12(1), 547–569. https://doi.org/10.1080/21505594.2021.1878688 DOI: https://doi.org/10.1080/21505594.2021.1878688
Deb, R., Kumar, A., Chakraborty, S., Verma, A. K., Tiwari, R., Dhama, K., Singh, U., & Kumar, S. (2013). Trends in diagnosis and control of bovine mastitis: A review. Pakistan Journal of Biological Sciences, 16(23), 1653–1661. https://doi.org/10.3923/ pjbs.2013.1653.1661 DOI: https://doi.org/10.3923/pjbs.2013.1653.1661
Dorcheh, F. A., Balmeh, N., & Sanjari, S. (2022). In-silico investigation of antibacterial herbal compounds in order to find new antibiotic against Staphylococcus aureus and its resistant subtypes. Informatics in Medicine Unlocked, 28, 100843. https://doi.org/10.1016/j.imu.2021.100843 DOI: https://doi.org/10.1016/j.imu.2021.100843
Emran, T. Bin, Rahman, M. A., Uddin, M. M. N., Dash, R., Hossen, M. F., Mohiuddin, M., & Alam, M. R. (2015). Molecular docking and inhibition studies on the interactions of Bacopa monnieri’s potent phytochemicals against pathogenic Staphylococcus aureus. DARU, Journal of Pharmaceutical Sciences, 23(1), 26. https://doi.org/10.1186/s40199-015-0106-9 DOI: https://doi.org/10.1186/s40199-015-0106-9
Goda, K., Kenzaka, T., Hoshijima, M., Yachie, A., & Akita, H. (2021). Toxic shock syndrome with a cytokine storm caused by Staphylococcus simulans: a case report. BMC Infectious Diseases, 21(1), 19. https://doi.org/10.1186/s12879-020-05731-y DOI: https://doi.org/10.1186/s12879-020-05731-y
Guo, Y., Song, G., Sun, M., Wang, J., & Wang, Y. (2020). Prevalence and Therapies of Antibiotic-Resistance in Staphylococcus aureus. Frontiers in Cellular and Infection Microbiology, 10, 107. https://doi.org/10.3389/fcimb.2020.00107 DOI: https://doi.org/10.3389/fcimb.2020.00107
Halasa, T., Huijps, K., Østerås, O., & Hogeveen, H. (2007). Economic effects of bovine mastitis and mastitis management: A review. Veterinary Quarterly, 29(1), 18–31. https://doi.org/ 10.1080/01652176.2007.9695224 DOI: https://doi.org/10.1080/01652176.2007.9695224
Harkins, C. P., Pichon, B., Doumith, M., Parkhill, J., Westh, H., Tomasz, A., de Lencastre, H., Bentley, S. D., Kearns, A. M., & Holden, M. T. G. (2017). Methicillin-resistant Staphylococcus aureus emerged long before the introduction of methicillin into clinical practice. Genome Biology, 18(1). https://doi.org/10.1186/ s13059-017-1252-9 DOI: https://doi.org/10.1186/s13059-017-1252-9
Hennekinne, J. A., De Buyser, M. L., & Dragacci, S. (2012). Staphylococcus aureus and its food poisoning toxins: characterization and outbreak investigation. FEMS Microbiology Reviews, 36(4), 815–836. https://doi.org/10.1111/J.1574-6976.2011.00311.X DOI: https://doi.org/10.1111/j.1574-6976.2011.00311.x
Huvenne, W., Hellings, P. W., & Bachert, C. (2013). Role of staphylococcal superantigens in airway disease. International Archives of Allergy and Immunology, 161(4), 304–314. https://doi.org/10.1159/000350329 DOI: https://doi.org/10.1159/000350329
Jayaram, B., Singh, T., Mukherjee, G., Mathur, A., Shekhar, S., & Shekhar, V. (2012). Sanjeevini: a freely accessible web-server for target directed lead molecule discovery. BMC Bioinformatics, 13 Suppl 1(Suppl 17). https://doi.org/10.1186/1471-2105-13-S17-S7 DOI: https://doi.org/10.1186/1471-2105-13-S17-S7
Kumar, A. S., Fernandes, N. J., Lobo, S. J., & Khan, N. (2022). In silico analysis of seaweed phytochemical flavonoid for the inhibition of staphylococcus enterotoxin A. Innovare Journal of Medical Sciences, 17–20. https://doi.org/10.22159/ ijms.2022.v10i4.45116 DOI: https://doi.org/10.22159/ijms.2022.v10i4.45116
Kurjogi, M., Satapute, P., Jogaiah, S., Abdelrahman, M., Daddam, J. R., Ramu, V., & Tran, L. S. P. (2018). Computational modeling of the staphylococcal enterotoxins and its interaction with natural antitoxin compounds. International Journal of Molecular Sciences, 19(1), 133. https://doi.org/10.3390/ijms19010133 DOI: https://doi.org/10.3390/ijms19010133
Li, J., Yang, J., Lu, Y. W., Wu, S., Wang, M. R., & Zhu, J. M. (2015). Possible role of staphylococcal enterotoxin b in the pathogenesis of autoimmune diseases. Viral Immunology, 28(7), 354–359. https://doi.org/10.1089/vim.2015.0017 DOI: https://doi.org/10.1089/vim.2015.0017
Lin, C. F., Chen, C. L., Huang, W. C., Cheng, Y. L., Hsieh, C. Y., Wang, C. Y., & Hong, M. Y. (2010). Different types of cell death induced by Enterotoxins. Toxins, 2(8), 2158–2176. https://doi.org/10.3390/toxins2082158 DOI: https://doi.org/10.3390/toxins2082158
Lin, Y. C., & Peterson, M. L. (2010). New insights into the prevention of Staphylococcal infections and toxic shock syndrome. Expert Review of Clinical Pharmacology, 3(6), 753. https://doi.org/10.1586/ECP.10.121 DOI: https://doi.org/10.1586/ecp.10.121
Lipinski, C. A. (2004). Lead- and drug-like compounds: the rule-of-five revolution. Drug Discovery Today. Technologies, 1(4), 337–341. https://doi.org/10.1016/J.DDTEC.2004.11.007 DOI: https://doi.org/10.1016/j.ddtec.2004.11.007
Loiselle, M. C., Ster, C., Talbot, B. G., Zhao, X., Wagner, G. F., Boisclair, Y. R., & Lacasse, P. (2009). Impact of postpartum milking frequency on the immune system and the blood metabolite concentration of dairy cows. Journal of Dairy Science, 92(5), 1900–1912. https://doi.org/10.3168/jds.2008-1399 DOI: https://doi.org/10.3168/jds.2008-1399
Mohana, R., & Venugopal, S. (2017). In silico Analysis of Toxins of Staphylococcus aureus for Validating Putative Drug Targets. Infectious Disorders - Drug Targets, 17(2), 130–142. https://doi.org/10.2174/1871526516666161230150219 DOI: https://doi.org/10.2174/1871526516666161230150219
O’Boyle, N. M., Banck, M., James, C. A., Morley, C., Vandermeersch, T., & Hutchison, G. R. (2011). Open Babel: An Open chemical toolbox. Journal of Cheminformatics, 3(10), 33. https://doi.org/10.1186/1758-2946-3-33 DOI: https://doi.org/10.1186/1758-2946-3-33
Rose, W., Fantl, M., Geriak, M., Nizet, V., & Sakoulas, G. (2021). Current Paradigms of Combination Therapy in Methicillin-Resistant Staphylococcus aureus (MRSA) Bacteremia: Does it Work, Which Combination, and For Which Patients? Clinical Infectious Diseases, 73(12), 2353–2360. https://doi.org/10.1093/ cid/ciab452 DOI: https://doi.org/10.1093/cid/ciab452
Selvaraj, J. (2020). Molecular docking analysis of Enterotoxin I from Staphylococcus aureus with Nafcillin analogues. Bioinformation, 16(10), 731–735. https://doi.org/10.6026/ 97320630016731 DOI: https://doi.org/10.6026/97320630016731
Sharun, K., Dhama, K., Tiwari, R., Gugjoo, M. B., Iqbal Yatoo, M., Patel, S. K., Pathak, M., Karthik, K., Khurana, S. K., Singh, R., Puvvala, B., Amarpal, Singh, R., Singh, K. P., & Chaicumpa, W. (2021). Advances in therapeutic and managemental approaches of bovine mastitis: a comprehensive review. The Veterinary Quarterly, 41(1), 107–136. https://doi.org/10.1080/ 01652176.2021.1882713 DOI: https://doi.org/10.1080/01652176.2021.1882713
Shidiki, A., & Vyas, A. (2022). Molecular docking and pharmacokinetic prediction of phytochemicals from Syzygium cumini in interaction with penicillin-binding protein 2a and erythromycin ribosomal methylase of Staphylococcus aureus. Biotechnologia, 103(1), 5–18. https://doi.org/10.5114/ bta.2022.113910 DOI: https://doi.org/10.5114/bta.2022.113910
Tuli, H. S., Bhatia, G. K., Sood, S., Debnath, P., Aggarwal, D., & Upadhyay, S. K. (2021a). In silico analysis and molecular docking studies of plumbagin and piperine ligands as potential inhibitors of alpha-glucosidase receptor. Biointerface Research in Applied Chemistry, 11(2), 9629–9637. https://doi.org/10.33263/ BRIAC112.96299637 DOI: https://doi.org/10.33263/BRIAC112.96299637
Tuli, H. S., Garg, V. K., Kapoor, D., Bansal, P., Kumar, P., Mohapatra, R. K., Dhama, K., Vashishth, A., Seth, P., & Bhatia, G. K. (2022). In silico targeting of osmoporin protein of Salmonella to identify anti-Salmonellosis phyto-compounds. Journal of Experimental Biology and Agricultural Sciences, 10(2), 423–429. https://doi.org/10.18006/2022.10(2).423.429 DOI: https://doi.org/10.18006/2022.10(2).423.429
Tuli, H. S., Sood, S., & Upadhyay, S. K. (2021b). In silico Molecular Docking of α-Glucosidase with Prangenidin and Columbin As An Anti-Hyperglycemic Strategy. Bioscience Biotechnology Research Communications, 14(3), 1191–1197. https://doi.org/10.21786/bbrc/14.3.43 DOI: https://doi.org/10.21786/bbrc/14.3.43
Zhou, K., Li, C., Chen, D., Pan, Y., Tao, Y., Qu, W., Liu, Z.,
Wang, X., & Xie, S. (2018). A review on nanosystems as an effective approach against infections of Staphylococcus aureus. International Journal of Nanomedicine Dovepress, 13, 7333–7347. https://doi.org/10.2147/IJN.S169935 DOI: https://doi.org/10.2147/IJN.S169935
Downloads
Published
How to Cite
License
Copyright (c) 2023 Journal of Experimental Biology and Agricultural Sciences

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.