A Review on DNA Vaccines in Pre-Clinical Trials Against SARS-CoV-2
DOI:
https://doi.org/10.18006/2022.10(3).487.493Keywords:
Covid-19, Vaccines, DNA vaccines, Clinical trialsAbstract
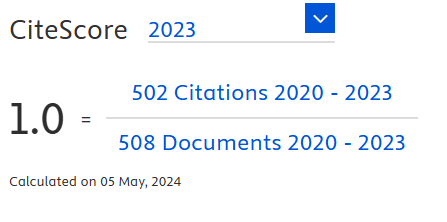
COVID 19 Pandemic is caused by the viral pathogen severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). Scientific fraternity worldwide swiftly developed various types of vaccines for the prevention and as mitigation measures for curbing the pandemic. Traditional inactivated vaccines, mRNA vaccines (protein subunits such as spike proteins), and viral vector vaccines (non-replicating vectors with protein subunits) have been approved by World Health Organisation (WHO) for emergency use. The emergence of many mutated variants has been a worrying factor in the fight against the pandemic. There has been continuous research in the quest for more therapeutics, especially vaccines to curb and stop the pandemic. According to WHO, there are 194 vaccines in pre-clinical trials belonging to various types out of which sixteen is DNA vaccines. In this review, we have discussed the advantages and disadvantages of the DNA vaccines for Covid - 19. This article tried to explore the available information on DNA vaccines and their current status against Covid – 19 which are in pre-clinical trials.
References
Abdo Hasson, S.S.A., Al-Busaidi, J.K.Z., & Sallam, T.A. (2015). The past, current and future trends in DNA vaccine immunisations. Asian Pacific Journal of Tropical Biomedicine, 5(5), 344-353. https://doi.org/10.1016/S2221-1691(15)30366-X. DOI: https://doi.org/10.1016/S2221-1691(15)30366-X
Abdulhaqq, S.A., & Weiner, D.B. (2008). DNA vaccines: developing new strategies to enhance immune responses. Immunologic Research, 42, 219. https://doi.org/10.1007/s12026-008-8076-3. DOI: https://doi.org/10.1007/s12026-008-8076-3
Abdurrahman, T., Aslihan A. G., & Marco M.C. (2020). COVID-19, immune system response, hyperinflammation and repurposing antirheumatic drugs. Turkish Journal of Medical Sciences, 50, 620-632. doi:10.3906/sag-2004-168. DOI: https://doi.org/10.3906/sag-2004-168
Ahmet, K.A., Mübeccel A., Dilek, A., et al. (2020). Immune response to SARS-CoV-2 and mechanisms of immunopathological changes in COVID-19. European Journal of Allergy and clinical immunology, 75(7), 1564-1581. https://doi.org/10.1111/all.14364. DOI: https://doi.org/10.1111/all.14364
Alexandra, C.W., Young-Jun, P., Alejandra T. M., et al. (2020). Structure, Function, and Antigenicity of the SARS-CoV-2 Spike Glycoprotein. Cell, 181(2), 281-292. https://doi.org/ 10.1016/j.cell.2020.02.058. DOI: https://doi.org/10.1016/j.cell.2020.02.058
Corbett, K.S., Flynn, B., Foulds, K.E., et al. (2020). Evaluation of the mRNA-1273 Vaccine against SARS-CoV-2 in Nonhuman Primates. New England Journal of Medicine, 383(16), 1544-1555. doi:10.1056/NEJMoa2024671. DOI: https://doi.org/10.1056/NEJMoa2024671
Coronaviridae Study Group of the International Committee on Taxonomy of Viruses. (2020). The species severe acute respiratory syndrome-related coronavirus: classifying 2019-nCoV and naming it SARS-CoV-2. Natural Microbiology, 5, 536-544. https://doi.org/10.1038 /s41564-020-0695-z. DOI: https://doi.org/10.1038/s41564-020-0695-z
Covidvax. (2020b). December, Retrieved from https://covidvax.org/covid19-vaccine/ Chula VRC/DNA-with-electroporation-Chula-Vaccine-Research-Center-National-Research-Council -of-Thailand-BioNet.
Covidvax. (2021a). December, Retrieved from https:// covidvax.org/covid19-vaccine/ ImmunomicEpivax/DNA-plasmid-needle-free-Immunomic-Tx-EpiVax-PharmaJet.
Covidvax. (2021b). October, Retrieved from https://covidvax.org/ covid19-vaccine/ Waterloo Uni/DN Mediphage-Bioceuticals-University-of-Waterloo-Lambton-College
CovidVax. (2020a) December Retrieved from https://covidvax.org/covid19-vaccine/Karolinska/DNA-with-electroporation-Karolinska-Institute-OpenCorona-EU-project-Folkh-lsomyndigheten-Igea-Cobra-.
CovidVax. (2021c). September update, Retrieved fromhttps://covidvax.org/covid19-vaccine/ EntosPharma/DNA-Entos-Pharma-Cytiva.
Cubuk, J., Alston, J.J., Incicco, J.J. et al. (2021). The SARS-CoV-2 nucleocapsid protein is dynamic, disordered, and phase separates with RNA. Nature Communication, 12, 1936. https:// doi.org/10.1038/s41467-021-21953-3. DOI: https://doi.org/10.1038/s41467-021-21953-3
Ebony, N., & David, B.W. (2020). DNA vaccines: prime time is now. Current Opinion in Immunology, 65, 21-27. https://doi.org/10.1016/j.coi.2020.01.006. DOI: https://doi.org/10.1016/j.coi.2020.01.006
FDA news. (2020). UK Pharma Company Scancell Selects COVID-19 Vaccine for Clinical Trials. December 2020, Retrieved from https://www.fdanews.com/articles/200556-uk-pharma-company-scancell-selects-covid-19-vaccine-for-clinical-trials.
Finkel, Y., Mizrahi, O., Nachshon, A., et al. (2021). The coding capacity of SARS-CoV-2. Nature, 589, 125-130. https://doi.org/ 10.1038/s41586-020-2739-1 DOI: https://doi.org/10.1038/s41586-020-2739-1
Giuseppina, M., Farthing, R.J., Lale-Farjat, S.L.M., & Bergeron J.R.C. (2020). Structural Characterization of SARS-CoV-2: Where We Are, and Where We Need to Be. Frontiers in Molecular Biosciences, 7, 605236. https://doi.org/10.3389/fmolb.2020.605236. DOI: https://doi.org/10.3389/fmolb.2020.605236
Gordon, D.E., Jang, G.M., Bouhaddou, M., et al. (2020). A SARS-CoV-2 protein interaction map reveals targets for drug repurposing. Nature, 583, 459-468. https://doi.org/10.1038/s 41586-020-2286-9.
Gustaf, A., Lars, F., Negin. N., et al. (2020). The SARS-CoV-2 N Protein is a Good Component in a Vaccine. Journal of Virology, 94(18), e01279-20. https://doi.org/10.1128 /JVI.01279-20. DOI: https://doi.org/10.1128/JVI.01279-20
Huang, Y., Yang, C., Xu, X.F., et al. (2020). Structural and functional properties of SARS-CoV-2 spike protein: potential antivirus drug development for COVID-19. Acta Pharmacologica Sinica, 41, 1141-1149. https://doi.org/10.1038/s41401-020-0485-4. DOI: https://doi.org/10.1038/s41401-020-0485-4
International Code of Virus Classification and Nomenclature. (2020) Retrieved from https://talk.ictvonline.org/information/w/ictv-information/383/ictv-code
Jordan, S.C. (2021). Innate and adaptive immune responses to SARS-CoV-2 in humans: relevance to acquired immunity and vaccine responses. Clinical and Experimental Immunology, 204(3), 310–320. https://doi.org/10.1111/cei.13582. DOI: https://doi.org/10.1111/cei.13582
Kowalczyk, D.W., & Ertl, H.C.J. (1999). Immune responses to DNA vaccines. Cellular and Molecular Life Sciences CMLS, 55, 751-770 (1999). https://doi.org/10.1007/s000180050330. DOI: https://doi.org/10.1007/s000180050330
Leo Y.Y.L., Leonard, I., & Aeron, C. H. (2018). A Review of DNA Vaccines Against Influenza. Frontiers in Immunology, 9, 1568. https://doi.org/10.3389/fimmu.2018.01568. DOI: https://doi.org/10.3389/fimmu.2018.01568
Liu, M.A. (2003), DNA vaccines: a review. Journal of Internal Medicine, 253, 402-410. https://doi.org/10.1046/j.1365-2796.2003.01140.x. DOI: https://doi.org/10.1046/j.1365-2796.2003.01140.x
Mohamadian, M., Chiti, H., Shoghli, A., Biglari, S., Parsamanesh, N., & Esmaeilzadeh, A. (2021). COVID-19: Virology, biology and novel laboratory diagnosis. The journal of gene medicine, 23(2), e3303. https://doi.org/10.1002/jgm.3303 DOI: https://doi.org/10.1002/jgm.3303
Meyers, L. M., Gutiérrez, A. H., Boyle, C. M., Terry, F., et al. (2021). Highly conserved, non-human-like, and cross-reactive SARS-CoV-2 T cell epitopes for COVID-19 vaccine design and validation. NPJ vaccines, 6(1), 71. https://doi.org/10.1038/s41541-021-00331-6 DOI: https://doi.org/10.1038/s41541-021-00331-6
Michael, M., Geraldine O. H. Catherine, H., et al. (2021). Severe Acute Respiratory Syndrome Coronavirus 2. Reference Module in Biomedical Sciences. Doi: 10.1016/B978-0-08-102723-3.00139-6. DOI: https://doi.org/10.1016/B978-0-08-102723-3.00139-6
Miyuki, K., Michiyo, K., Kazuya, S., & Shutoku, M. (2019). Biochemical Analysis of Coronavirus Spike Glycoprotein Conformational Intermediates during Membrane Fusion. Journal of Virology, 93(19), e00785-19. https://doi.org/10.1128/JVI.00785-19. DOI: https://doi.org/10.1128/JVI.00785-19
Narayanan, K., Huang, C., & Makino, S. (2008). SARS coronavirus accessory proteins. Virus Research, 133 (1), 133-121. https://doi.org/10.1016/j.virusres.2007.10.009. DOI: https://doi.org/10.1016/j.virusres.2007.10.009
New, University of Cambridge, August. (2020). University of Cambridge to trial Covid-19 vaccine candidate, Clinical trials arena. Retrieved from https://www.clinicaltrialsarena.com /news/cambridge-uni-covid-vaccine/.
Press Release, (March 31st, 2020). MediphageBioceuticals, Press Release 2020, March 31 MediphageBioceuticals, Inc. Initiates a COVID-19 Vaccine Development Program, Retrieved from https://static1.squarespace.com/static/5cab96df2727be742dcf64ac/t/5efdf1b534e269 1d9e3ef002/1593700790604/COVID19+Press +Release%2805.15.2020%29.V2+%28New +L ayout%29-2.pdf.
Press Release. (1st September, 2021). Entos Pharma, Entos’ COVID-19 DNA Vaccine Candidate Approved for Phase 2 Clinical Trial in South Africa, Retrieved from https://www.entospharma. com/news/entos-covid-19-dna-vaccine-candidate-approved-for-phase-2-clinical-trial-in-south -africa.
Prompetchara, E., Ketloy, C., Tharakhet, K., Kaewpang, P., et al. (2021). DNA vaccine candidate encoding SARS-CoV-2 spike proteins elicited potent humoral and Th1 cell-mediated immune responses in mice. PloS one, 16(3), e0248007. https://doi.org/10.1371/journal.pone.0248007. DOI: https://doi.org/10.1371/journal.pone.0248007
Rota, P. A., Oberste, M. S., Monroe, S. S., Nix, W. A., et al. (2003). Characterization of a novel coronavirus associated with severe acute respiratory syndrome. Science (New York, N.Y.), 300 (5624), 1394–1399. https://doi.org/10.1126/science.1085952. DOI: https://doi.org/10.1126/science.1085952
Sarkar, M., & Saha, S. (2020). Structural insight into the role of novel SARS-CoV-2 E protein: A potential target for vaccine development and other therapeutic strategies. PloS one, 15(8), e0237300. https://doi.org/10.1371/journal.pone.0237300. DOI: https://doi.org/10.1371/journal.pone.0237300
Scancell Holdings plc. (2020), Scancell announces selection of COVID-19 vaccine candidate, SN14 Retrieved from https://www.scancell.co.uk/Data/Sites/1/media/ publications/ rns/covid-19-vaccine-candidate-selected.pdf). updated in Covidvax, December 2020, https://covidvax .org/covid19-vaccine/Scancell/DNA-Scancell-University-of-Nottingha m-Nottingham-Trent-University.
Schoeman, D., & Fielding, B. C. (2019). Coronavirus envelope protein: current knowledge. Virology journal, 16(1), 69. https://doi.org/10.1186/s12985-019-1182-0 DOI: https://doi.org/10.1186/s12985-019-1182-0
Shah, V. K., Firmal, P., Alam, A., Ganguly, D., & Chattopadhyay, S. (2020). Overview of Immune Response During SARS-CoV-2 Infection: Lessons From the Past. Frontiers in immunology, 11, 1949. https://doi.org/10.3389/fimmu.2020.01949. DOI: https://doi.org/10.3389/fimmu.2020.01949
Silvas, J. A., Vasquez, D. M., Park, J. G., Chiem, K., et al. (2021). Contribution of SARS-CoV-2 Accessory Proteins to Viral Pathogenicity in K18 Human ACE2 Transgenic Mice. Journal of virology, 95(17), e0040221. https://doi.org/10.1128/JVI.00402-21. DOI: https://doi.org/10.1128/JVI.00402-21
Stachyra, A., Góra-Sochacka, A., & Sirko, A. (2014). DNA vaccines against influenza. Acta Biochimica Polonica, 61(3), 515-522. DOI: https://doi.org/10.18388/abp.2014_1873
Surjit, M., & Lal, S. K. (2009). The Nucleocapsid Protein of the SARS Coronavirus: Structure, Function and Therapeutic Potential. Molecular Biology of the SARS-Coronavirus, 129–151. https://doi.org/10.1007/978-3-642-03683-5_9. DOI: https://doi.org/10.1007/978-3-642-03683-5_9
U.S. National Library of Medicine. (2021). A Clinical Trial of a Prophylactic Plasmid DNA Vaccine for COVID-19 [Covigenix VAX-001] in adults. September 14, Retrieved from https://clinicaltrials.gov/ct2/show/NCT04591184).
van Doremalen, N., Lambe, T., Spencer, A., Belij-Rammerstorfer, S., et al. (2020). ChAdOx1 nCoV-19 vaccine prevents SARS-CoV-2 pneumonia in rhesus macaques. Nature, 586(7830), 578–582. https://doi.org/10.1038/s41586-020-2608-y. DOI: https://doi.org/10.1038/s41586-020-2608-y
Wang, H., Zhang, Y., Huang, B., Deng, W., et al. (2020). Development of an Inactivated Vaccine Candidate, BBIBP-CorV, with Potent Protection against SARS-CoV-2. Cell, 182(3), 713–721.e9. https://doi.org/10.1016/j.cell.2020.06.008. DOI: https://doi.org/10.1016/j.cell.2020.06.008
Wu, F., Zhao, S., Yu, B., Chen, Y. M., et al. (2020). A new coronavirus associated with human respiratory disease in China. Nature, 579 (7798), 265–269. https://doi.org/10.1038/ s41586-020-2008-3. DOI: https://doi.org/10.1038/s41586-020-2008-3
Xaquin, C. D., Sebastian, O., Karin, L., & Gunilla, B. K. H. (2020). Immunity to SARS-CoV-2 induced by infection or vaccination. Journal of Internal Medicine, 291(1), 32-50. https://doi.org/10.1111/joim.13372. DOI: https://doi.org/10.1111/joim.13372
Yadav, R., Chaudhary, J. K., Jain, N., Chaudhary, P. K., et al. (2021). Role of Structural and Non-Structural Proteins and Therapeutic Targets of SARS-CoV-2 for COVID-19. Cells, 10(4), 821. https://doi.org/10.3390/cells10040821. DOI: https://doi.org/10.3390/cells10040821
Downloads
Published
How to Cite
Issue
Section
License

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.