Role of Probiotic Microorganisms in the Brain Plasticity Development
DOI:
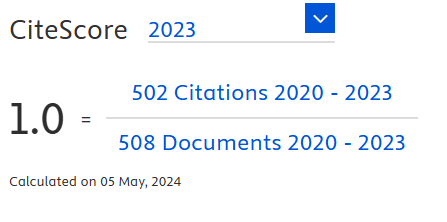
https://doi.org/10.18006/2024.12(3).354.365Keywords:
Cognition, Synaptic Plasticity, Probiotics, Reward-based learning paradigmAbstract
Probiotics are defined as beneficial microorganisms that are responsible for the maintenance of homeostasis mechanisms within the host system, especially in humans. Other than homeostasis, it is also used to improve a host system's cognition, immune functions, and antioxidant levels. Over the past decades, probiotic microorganisms have been used most commonly as traditional fermented foods in our country and some parts of southeast asia. These fermented food products majorly consist of Lactobacillus species, including Lactobacillus acidophilus, L. fermentum, and L. plantarum. The present study explored the potential role of three different lactobacillus strains (L. acidophilus, L. fermentum, and L. Plantarum) in forming brain plasticity changes (BPC) with the help of a cue-based learning paradigm (CBLP). Two staged behavioral studies were conducted for all behavioral analysis groups (BAG) before (without probiotic infusions - WiPI) and after probiotic infusions (with probiotic infusions - WPI) in RBLP. Behavioral responses of the WiPI & WPI phases showed the effect of a stress-free habituated environment in developing BPC and strengthening of BPC by oral infusions of probiotic microorganisms (PM). WiPI and WPI behavioral analysis were used in this study to validate BPC in a laboratory-controlled environment. Infusion of probiotic microorganisms through oral passage may have a more significant impact on the synthesis, production, and transmission of neurotransmitter precursor compounds (NPC) from the gut to the central nervous system (CNS) through the blood-brain barrier (BBB). Increased transmission of the NPC strengthens the formed plasticity changes, which results in the formation of cognitive memory functions. Thus, the present study proved that probiotic microorganisms may play a major role in cognition development through the BPC.
References
Abraham, W.C., Jones, O.D., & Glanzman, D.L. (2019). Is plasticity of synapses the mechanism of long-term memory storage? Npj Science of Learning, 4, 9. DOI: https://doi.org/10.1038/s41539-019-0048-y
Ahmed, G.K., Ramadan, H.K., Elbeh, K., & Haridy, N.A. (2024). Bridging the gap: associations between gut microbiota and psychiatric disorders. Middle East Current Psychiatry, 31, 2. DOI: https://doi.org/10.1186/s43045-024-00395-9
Alajangi, H.K., Kaur, M., Sharma, A., Rana, S., et al. (2022). Blood-brain barrier: emerging trends on transport models and new-age strategies for therapeutics intervention against neurological disorders. Molecular Brain, 15, 49. DOI: https://doi.org/10.1186/s13041-022-00937-4
Appelbaum, L.G., Shenasa, M.A., Stolz, L., & Daskalakis, Z. (2023). Synaptic plasticity and mental health: methods, challenges and opportunities. Neuropsychopharmacology, 48, 113-120. DOI: https://doi.org/10.1038/s41386-022-01370-w
Appleton, J. (2018). The Gut-brain Axis: Influence of Microbiota on Mood and Mental Health. Integrative Medicine, 17, 28-32.
Ashok, A., Leroy, F., Rayman, J.B., & Kandel, E.R. (2019). Molecular Mechanisms of the Memory Trace. Trends in Neuroscience, 42, 14-22. DOI: https://doi.org/10.1016/j.tins.2018.10.005
Bai, Y., & Suzuki, T. (2020). Activity-Dependent Synaptic Plasticity in Drosophila melanogaster. Frontiers in physiology, 11, 161. DOI: https://doi.org/10.3389/fphys.2020.00161
Chaudhry, T.S., Senapati, S.G., Gadam, S., Mannam, H.P.S.S., et al. (2023). The Impact of Microbiota on the Gut-brain Axis: Examining the complex Interplay and Implications. Journal of Clinical Medicine, 12, 5231. DOI: https://doi.org/10.3390/jcm12165231
Chaudhury, S., Sharma, V., Kumar, V., Nag, T.C., & Wadhwa, S. (2016). Activity-dependent synaptic plasticity modulates the critical phase of brain development. Brain & Development, 38, 355-363. DOI: https://doi.org/10.1016/j.braindev.2015.10.008
Chen, D., Yang, X., Yang, J., Lai, G., et al. (2017). Prebiotic effect of fructooligosaccharides from Morinda officinalis on alzheimer's disease in rodent models by targeting the microbiota-gut-brain axis. Frontiers in Aging Neuroscience, 9, 403. DOI: https://doi.org/10.3389/fnagi.2017.00403
Chen, Y., Xu, J., & Chen, Y. (2021). Regulation of Neurotransmitters by the Gut Microbiota and Effects on Cognition in Neurological Disorders. Nutrients, 13, 2099. DOI: https://doi.org/10.3390/nu13062099
Dahiya, D., & Nigam, P.S. (2022). The Gut Microbiota Influenced by the Intake of Probiotics and Functional Foods with Prebiotics Can Sustain Wellness and Alleviate Certain Ailments like Gut-Inflammation and Colon-Cancer. Microorganisms, 10, 665. DOI: https://doi.org/10.3390/microorganisms10030665
Dash, S., Syed, Y.A., & Khan, M.R. (2022). Understanding the Role of the Gut Microbiome in Brain Development and Its Association With Neurodevelopmental Psychiatric Disorders. Frontiers in Cell and Developmental Biology, 10, 880544. DOI: https://doi.org/10.3389/fcell.2022.880544
Den, H., Dong, X., Chen, M., & Zhou, Z. (2020). Efficacy of probiotics on cognition, and biomarkers of inflammation and oxidative stress in adults with Alzheimer's disease or mild cognitive impairment – a meta-analysis of randomized controlled trials. Aging, 12, 4010-4039. DOI: https://doi.org/10.18632/aging.102810
Dicks, L.M.T. (2022). Gut Bacteria and Neurotransmitters. Microorganisms, 10, 1838. DOI: https://doi.org/10.3390/microorganisms10091838
Evans, H.T., Blackmore, D., Götz, J., & Bodea, L. (2021). De novo proteomic methods for examining the molecular mechanisms underpinning long-term memory. Brain Research Bulletin, 169, 94-103. DOI: https://doi.org/10.1016/j.brainresbull.2020.12.015
Freimer, D., Yang, T.T., Ho, T.C., Tymofiyeva, O., & Leung, C. (2022). The gut microbiota, HPA axis, and brain in adolescent-onset depression: Probiotics as a novel treatment. Brain, Behaviour, & Immunity, 26, 100541. DOI: https://doi.org/10.1016/j.bbih.2022.100541
Ganesh, A., Bogdanowicz, W., Balamurugan, K., Varman, D.R., & Rajan, K.E. (2012). Egr-1 antisense oligodeoxynucleotide administration into the olfactory bulb impairs olfactory learning in the greater short-nosed fruit bat Cynopterus sphinx. Brain Research, 1471, 33-45. DOI: https://doi.org/10.1016/j.brainres.2012.06.038
Ganesh, A., Bogdanowicz, W., Haupt, M., Marimuthu, G., & Rajan, K.E. (2010). Role of olfactory bulb serotonin in olfactory learning in the greater short-nosed fruit bat, Cynopterus sphinx (Chiroptera: Pteropodidae). Brain Research, 1352, 108-117. DOI: https://doi.org/10.1016/j.brainres.2010.06.058
Gebrayel, P., Nicco, C., Khodor, A.A., Bilinski, J., et al. (2022). Microbiota medicine: towards clinical revolution. Journal of Translational Medicine, 20, 111. DOI: https://doi.org/10.1186/s12967-022-03296-9
Gentile, C.L., & Weir, T.L. (2018). The gut microbiota at the intersection of diet and human health. Science, 362, 776-780. DOI: https://doi.org/10.1126/science.aau5812
Han, S., Lu, Y., Xie, J., Fei, Y., et al. (2021). Probiotic Gastrointestinal Transit and Colonization After Oral Administration: A Long Journey. Frontiers in Cellular and Infection Microbiology, 11, 609722. DOI: https://doi.org/10.3389/fcimb.2021.609722
Hillemacher, T., Bachmann, O., Kahl, K.G., & Frieling, H. (2018). Alcohol, microbiome, and their effect on psychiatric disorders. Progress in Neuropsychopharmacology and Biological Psychiatry, 85, 105-115. DOI: https://doi.org/10.1016/j.pnpbp.2018.04.015
Ji, J., Jin, W., Liu, S., Jiao, Z., & Li, X. (2023). Probiotics, probiotics, and postbiotics in health and disease. MedComm, 4, e420. DOI: https://doi.org/10.1002/mco2.420
Kandpal, M., Indari, O., Baral, B., Jakhmola, S., et al. (2022). Dysbiosis of Gut Microbiota from the Perspective of the Gut-Brain Axis: Role in the Provocation of Neurological Disorders. Metabolites, 12, 1064. DOI: https://doi.org/10.3390/metabo12111064
Kim, S., Kim, H., & Um, J.W. (2018). Synapse development organized by neuronal activity-regulated immediate-early genes. Experimental & Molecular Medicine, 50, 1-7. DOI: https://doi.org/10.1038/s12276-018-0025-1
Kumar, A., Sivamaruthi, B.S., Dey, S., Kumar, Y., Malviya, R., Prajapati, B.G., & Chaiyasut, C. (2024). Probiotics as modulators of gut-brain axis for cognitive development. Frontiers in Pharmacology, 15, 1348297. DOI: https://doi.org/10.3389/fphar.2024.1348297
Lin, H., Chen, C., de Belle, J.S., & Chiang, A. (2021). CREBA and CREBB in two identified neurons gate long-term memory formation in Drosophila. Proceedings of the National Academy of the United States of America, 118, e2100624118. DOI: https://doi.org/10.1073/pnas.2100624118
Liu, N., Yang, D., Sun, J., & Li, Y. (2023). Probiotic supplements are effective in people with cognitive impairment: a meta-analysis of randomized controlled trials. Nutrition Reviews, 81, 1091-1104. DOI: https://doi.org/10.1093/nutrit/nuac113
Luis, C.O.S., & Ryan, T.J. (2022). Understanding the physical basis of memory: Molecular mechanisms of the engram. Journal of Biological Chemistry, 298, 101866. DOI: https://doi.org/10.1016/j.jbc.2022.101866
Malik, J.A., Zafar, M.A., Lamba, T., Nanda, S., et al. (2023). The impact of aging-induced gut microbiome dysbiosis on dendritic cells and lung diseases. Gut Microbes, 15, 2290643. DOI: https://doi.org/10.1080/19490976.2023.2290643
Margoob, M., Kouser, S., & Jan, N. (2024). Serotonin: The Link between Gut Microbiome and Brain. In K.F. Shad (Ed), Serotonin – Neurotransmitter and Hormone of Brain. IntechOpen. DOI:10.5772/intechopen.1003826. DOI: https://doi.org/10.5772/intechopen.1003826
Miri, S., Yeo, J., Abubaker, S., & Hammami, R. (2023). Neuromicrobiology, an emerging neurometabolic facet of the gut microbiome? Frontiers in Microbiology, 14, 1098412. DOI: https://doi.org/10.3389/fmicb.2023.1098412
Misiak, B., Łoniewski, I., Marlicz, W., Freydeca, W., et al. (2020). The HPA axis dysregulation in severe mental illness: can we shift the blame to gut microbiota. Progress in Neuro Psychopharmacology and Biological Psychiatry, 102, 109951. DOI: https://doi.org/10.1016/j.pnpbp.2020.109951
Mitra, S., Dash, R., Nishan, A.A., Habiba, S.U., & Moon, I.S. (2023). Brain modulation by the gut microbiota: From disease to therapy. Journal of Advanced Research, 53, 153-173. DOI: https://doi.org/10.1016/j.jare.2022.12.001
Mukilan, M., Elakkiya, V., Darshini, M., & Varshini, M. (2024a). Exploring the Potential Role of Lactobacillus plantarum in the Reversal of Induced Cognitive Long-term Memory Impairment. Journal of Experimental Biology and Agricultural Sciences, 12, 175-187. DOI: https://doi.org/10.18006/2024.12(2).175.187
Mukilan, M., Antony Mathew, M.T., Yaswanth, S., & Mallikarjun, V. (2024b). Role of Probiotic Strain Lactobacillus acidophilus in the Reversal of Gut Dysbiosis Induced Brain Cognitive Decline. Journal of Experimental Biology and Agricultural Sciences, 12, 36-48. DOI: https://doi.org/10.18006/2024.12(1).36.48
Mukilan, M. (2023). Impact of Pseudomonas aeruginosa, Bacillus subtilis, Staphylococcus aureus, and Escherichia coli Oral Infusions on Cognitive Memory Decline in Mild Cognitive Impairment. Journal of Experimental Biology and Agricultural Sciences, 11, 581-592. DOI: https://doi.org/10.18006/2023.11(3).581.592
Mukilan, M. (2022). Effects of Probiotics, Prebiotics and Synbiotic Supplementation on Cognitive Impairment: A Review. Journal of Experimental Biology and Agricultural Sciences, 10, 1-11. DOI: https://doi.org/10.18006/2022.10(1).1.11
Mukilan, M., Bogdanowicz, W., Marimuthu, G., & Rajan, K.E. (2018a). Odour discrimination learning in the Indian greater short-nosed fruit bat (Cynopterus sphinx): differential expression of Egr-1, C-fos and PP-1 in the olfactory bulb, amygdala and hippocampus. Journal of Experimental Biology, 221, jeb175364. DOI: https://doi.org/10.1242/jeb.175364
Mukilan, M., Rajathei, D.M., Jeyaraj, E., Kayalvizhi, N., & Rajan, K.E. (2018b). MiR-132 regulated olfactory bulb proteins linked to olfactory learning in greater short-nosed fruit bat Cynopterus sphinx. Gene, 671, 10-20. DOI: https://doi.org/10.1016/j.gene.2018.05.107
Mukilan, M., Varman, D.R., Sudhakar, S., & Rajan, K.E. (2015). Activity-dependent expression of miR-132 regulates immediate early gene induction during olfactory learning in the greater short-nosed fruit bat, Cynopterus sphinx. Neurobiology of Learning and Memory, 120, 41-51. DOI: https://doi.org/10.1016/j.nlm.2015.02.010
Narengaowa, Kong, W., Lan, F., Awan, U.F., et al. (2021). The Oral-Gut-Brain AXIS: The Influence of Microbes in Alzheimer's Disease. Frontiers in Cellular Neuroscience, 15, 633735. DOI: https://doi.org/10.3389/fncel.2021.633735
Norris, D. (2017). Short-Term Memory and Long-Term Memory are Still Different. Psychological Bulletin, 143(9), 992-1009. DOI: https://doi.org/10.1037/bul0000108
O'Donnell, M.P., Fox, B.W., Chao, P., Schroder, F.C., & Sengupta, P. (2020). A neurotransmitter produced by gut bacteria modulates host sensory behaviour. Nature, 583, 415-420.
Ortega-Martínez, S. (2015). A new perspective on the role of the CREB family of transcription factors in memory consolidation via adult hippocampal neurogenesis. Frontiers in Molecular Neuroscience, 8, 46. DOI: https://doi.org/10.3389/fnmol.2015.00046
Paudel, D., Uehara, O., Giri, S., Yoshida, K., et al. (2022). Effect of psychological stress on the oral-gut microbiota and the potential oral-gut-brain axis. Japanese Dental Science Review, 58, 365-375. DOI: https://doi.org/10.1016/j.jdsr.2022.11.003
Peng, S., Zhang, Y., Zhang, J., Wang, H., & Ren, B. (2010). ERK in learning and memory: a review of recent research. International Journal of Molecular Sciences, 11, 222-232. DOI: https://doi.org/10.3390/ijms11010222
Pitchaikani, S., Mukilan, M., Govindan, P., Kathiravan G., Shakila H. (2024). Highlighting the Importance of Matrix Metalloproteinase 1, 8, and 9 Expression during the Progression of Mycobacterium tuberculosis Infection. Journal of Experimental Biology and Agricultural Sciences, 12, 49-59. DOI: https://doi.org/10.18006/2024.12(1).49.59
Rajan, K.E. (2021). Olfactory learning and memory in the greater short-nosed fruit bat Cynopterus sphinx: the influence of conspecifics distress calls. Journal of Comparative physiology. A, Neuroethology, Sensory, Neural, and Behavioral Physiology, 207, 667-679. DOI: https://doi.org/10.1007/s00359-021-01505-2
Ramirez, A., & Arbuckle, M.R. (2016). Synaptic Plasticity: The Role of Learning and Unlearning in Addiction and Beyond. Biological Psychiatry, 80(9), e73-e75. DOI: https://doi.org/10.1016/j.biopsych.2016.09.002
Sabit, H., Kassab, A., Alaa, D., Mohamed, D., et al. (2023). The Effect of Probiotic Supplementation on the Gut-Brain Axis in Psychiatric Patients. Current Issues in Molecular Biology, 45, 4080-4099. DOI: https://doi.org/10.3390/cimb45050260
Salami, M., & Soheili, M. (2022). The microbiota-gut-hippocampus axis. Frontiers in Neuroscience, 16, 1065995. DOI: https://doi.org/10.3389/fnins.2022.1065995
Sandhu, K.V., Sherwin, E., Schellekens, H., Stanton, C., et al. (2017). Feeding the microbiota-gut-brain axis: diet, microbiome, and neuropsychiatry. Translational Research, 179, 223-244. DOI: https://doi.org/10.1016/j.trsl.2016.10.002
Sarkar, A., Yoo, J.Y., Dutra, S.V.O., Morgan, K.H., & Groer, M. (2021). The Association between Early-Life Gut Microbiota and Long-Term Health and Diseases. Journal of Clinical Medicine, 10, 459. DOI: https://doi.org/10.3390/jcm10030459
Sarubbo, F., Cavallucci, V., & Pani, G. (2022). The Influence of Gut Microbiota on Neurogenesis: Evidence and Hopes. Cells, 11, 382. DOI: https://doi.org/10.3390/cells11030382
Savin, Z., Kivity, S., Yonath, H., & Yehuda, S. (2018). Smoking and the intestinal microbiome. Archives of Microbiology, 200, 677-684. DOI: https://doi.org/10.1007/s00203-018-1506-2
Sengupta, P. (2020). A neurotransmitter produced by gut bacteria modulates host sensory behaviour. Nature, 583, 415-420. DOI: https://doi.org/10.1038/s41586-020-2395-5
Suganya, K., & Koo, B. (2020). Gut-Brain Axis: Role of Gut Microbiota on Neurological Disorders and How Probiotics/Prebiotics Beneficially Modulate Microbial and Immune Pathways to Improve Brain Functions. International Journal of Molecular Sciences, 21, 7551. DOI: https://doi.org/10.3390/ijms21207551
Varela-Trinidad, G.U., Domínguez-Diaz, C., Solórzano-Castanedo, K., Íñiguez-Gutiérrez, L., et al. (2022). Probiotics: Protecting Our Health from the Gut. Microorganisms, 10, 1428. DOI: https://doi.org/10.3390/microorganisms10071428
Wang, X., Zhang, P., & Zhang, X. (2021). Probiotics Regulate Gut Microbiota: An Effective Method to Improve Immunity. Molecules, 26, 6076. DOI: https://doi.org/10.3390/molecules26196076
Yang, X., Yu, D., Xue, L., Li, H., et al. (2020). Probiotics modulate the microbiota-gut-brain axis and improve memory deficits in aged SAMP8 mice. Acta Pharmaceutica Sinicia B, 10, 475-87. DOI: https://doi.org/10.1016/j.apsb.2019.07.001
Zheng, D., Liwinski, T., & Elinay, E. (2020). Interaction between microbiota and immunity in health and disease. Cell Research, 30, 492-506. DOI: https://doi.org/10.1038/s41422-020-0332-7
Zhu, G., Zhao, J., Zhang, H., Chen, W., & Wang, G. (2021). Probiotics for Mild Cognitive Impairment and Alzheimer's Disease: A Systematic Review and Meta-Analysis. Foods, 10, 1672. DOI: https://doi.org/10.3390/foods10071672
Downloads
Published
How to Cite
License
Copyright (c) 2024 Journal of Experimental Biology and Agricultural Sciences

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.