AN ASSESSMENT OF PESTICIDE POISONING INCIDENCES PRESENTED AT HEALTH CARE FACILITIES IN MASHONALAND CENTRAL PROVINCE, ZIMBABWE
DOI:
https://doi.org/10.18006/2024.12(2).226.236Keywords:
HHPs, HCF, HCW, Poisoning, IncidenceAbstract
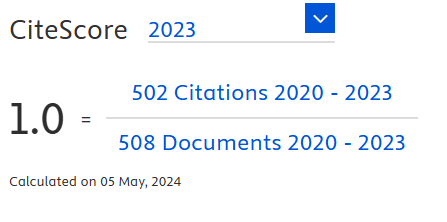
Acute Pesticide Poisoning (APP) is a significant problem in developing countries, causing loss of productivity and fatalities in the agricultural sector. However, limited information on the connection between pesticide use, APP, and deaths in Zimbabwe is available. This study aimed to evaluate incidents that resulted in APP and identify the specific pesticides that caused them at Health Care Facilities (HCFs) in Mashonaland Central Province. Researchers conducted a survey asking standardized questions to gather information on APP cases from 93 HCFs. Descriptive statistics and chi-square association tests for APP cases in the targeted HCFs were calculated using IBM SPSS version 22. The study found that 43% of APP cases were due to pesticides belonging to the World Health Organization (WHO) class II acute toxicity category, while 26.1% were caused by Highly Hazardous Pesticides (HHPs). Most of the cases were due to intentional poisoning (87.1%), with the majority (55.9%) of APP incidents being males. The highest APP cases were recorded in the 21-30 age group (38.8%), followed by the 31-40 age group (32.8%). These results emphasize the significant impact of intentional poisoning by WHO class II type pesticides, particularly HHPs, on the incidence of APP in Zimbabwe. To mitigate the impact of HHPs on human health, it is recommended that the government of Zimbabwe consider pesticide risk reduction measures, such as stricter pesticide registration criteria, import restrictions, and the promotion of less toxic alternatives. These findings highlight the urgent need for policymakers, researchers, and other stakeholders in the agricultural sector to work collaboratively towards creating a safer and more sustainable farming environment in Zimbabwe.
References
Bar, J., Bickel, U., Bollmohr, S., Bombardi, L. M., Bourgin, C., et al. (2022). Pesticide Atlas. In L. Tostado, & S. Bollmohr (eds.) Facts and figures about agricultural toxic chemicals (2nd ed). https://eu.boell.org/en/PesticideAtlas
Bayoumi, E. A. (2022). Deleterious Effects of Banned Chemical Pesticides on Human Health in Developing Countries. In M. L. Larramendy & S. Soloneski (Eds.) Pesticides - Updates on toxicity, efficacy and risk assessment (pp. 1–27). Intech Open Publisher DOI: 10.5772/intechopen.104571. DOI: https://doi.org/10.5772/intechopen.104571
Benaboud, J., Elachour, M., Oujidi, J., & Chafi, A. (2021). Farmer's behaviors toward pesticides use: insight from a field study in Oriental Morocco. Environmental analysis, health and toxicology, 36(1), e2021002. https://doi.org/10.5620/eaht.2021002 DOI: https://doi.org/10.5620/eaht.2021002
Boedeker, W., Watts, M., Clausing, P., & Marquez, E. (2020). The global distribution of acute unintentional pesticide poisoning: estimations based on a systematic review. BMC Public Health, 20 (1875), 1–19. https://doi.org/10.1186/s12889-020-09939-0 DOI: https://doi.org/10.1186/s12889-020-09939-0
Bradberry, S. M., Cage, S. A., Proudfoot, A. T., & Vale, A. J. (2005). Poisoning due to pyrethroids (Review Article). Toxicology Review National Poisons Information Service (Birmingham Centre), 24(2), 93–106. DOI: https://doi.org/10.2165/00139709-200524020-00003
Brassell, M., Karunarathne, A., Utyasheva, L., Eddleston, M., Konradsen, F., & Rother, H. A. (2022). Current pesticide suicide surveillance methods used across the African continent: A scoping review protocol. BMJ Open, 12(8), 1–8. https://doi.org/10.1136/ bmjopen-2021-055923 DOI: https://doi.org/10.1136/bmjopen-2021-055923
Buckley, N. A., Fahim, M., Raubenheimer, J., Gawarammana, I. B., Eddleston, M., Roberts, M. S., & Dawson, A. H. (2021). Case fatality of agricultural pesticides after self-poisoning in Sri Lanka: A prospective cohort study. The Lancet Global Health, 9(6), e854–e862. https://doi.org/10.1016/S2214-109X(21)00086-3 DOI: https://doi.org/10.1016/S2214-109X(21)00086-3
Chan, L. F., Chin, S. J., Loo, T. H., Panirselvam, R. R., Chang, S., et al. (2023). Surveillance of pesticide poisoning in an East and a West Malaysian hospital: Characteristics of pesticide poisoning and the early impact of a national Paraquat ban. BMC Psychiatry, 23(1), 1–13. https://doi.org/10.1186/s12888-023-04974-8 DOI: https://doi.org/10.1186/s12888-023-04974-8
Dorooshi, G., Mirzae, M., Fard, N., Zoofaghari, S., & Mood, N. (2021). Investigating the outcomes of aluminium phosphide poisoning in Khorshid referral hospital, Isfahan, Iran: A retrospective study. Journal of Research in Pharmacy Practice, 10(4), 166. https://doi.org/10.4103/jrpp.jrpp_88_21 DOI: https://doi.org/10.4103/jrpp.jrpp_88_21
Eizadi-Mood, N., Mahvari, R., Akafzadeh Savari, M., Mohammadbeigi, E., et al. (2023). Acute pesticide poisoning in the central part of Iran: A 4-year cross-sectional study. SAGE Open Medicine, 11, 1–11. https://doi.org/https://doi.org/10.1177/ 20503121221147352 DOI: https://doi.org/10.1177/20503121221147352
FAO/WHO. (2016). International Code of Conduct on Pesticide Management. Guidelines on Highly Hazardous Pesticides (Issue March). FAO Communication Division. Retrieved from https://www.fao.org/publications/card/en/c/a5347a39-c961-41bf-86a4-975cdf2fd063/
FAO/WHO. (2019). Preventing Suicide: A resource for pesticide registrars and regulators (pp. 1–36). Retrieved from http://www.fao.org/3/ca6027en/CA6027EN.pdf
Foti, R., & Chikuvire, T.(2005). Farm Level Pesticide Use and Productivity in Smallholder Cotton Production in Zimbabwe : The Case of Gokwe Communal Area Farmers (pp. 116–127). Retrieved from http://citeseerx.ist.psu.edu/viewdoc/download?doi=10.1.1. 543. 1312&rep=rep1&type=pdf
Freeman, A., Mergl, R., Kohls, E., Székely, A., Gusmao, R., et al. (2017). A cross-national study on gender differences in suicide intent. BMC Psychiatry, 17(1), 1–11. https://doi.org/10.1186/ s12888-017-1398-8 DOI: https://doi.org/10.1186/s12888-017-1398-8
Hurtado, D., Quintero, J. A., Rodríguez, Y. A., Pérez, D. E., Paz, R. F., & Diez-Sepúlveda, J. (2024). Principal causes of acute poisoning in an emergency service: experience between 2014 and 2021 at a University Hospital in Southwestern Colombia. Scientific Reports, 14(1), 1–11. https://doi.org/10.1038/s41598-024-54159-w DOI: https://doi.org/10.1038/s41598-024-54159-w
Jesslin, J., Adepu, R., & Churi, S. (2010). Assessment of prevalence and mortality incidences due to poisoning in a South Indian tertiary care teaching hospital. Indian Journal of Pharmaceutical Sciences, 72(5), 587–591. https://doi.org/10.4103/ 0250-474X.78525 DOI: https://doi.org/10.4103/0250-474X.78525
Jørs, E., Neupane, D., & London, L. (2018). Pesticide poisonings in low- and middle-income countries. Environmental Health Insights, 12, 1–3. https://doi.org/10.1177/1178630217750876 DOI: https://doi.org/10.1177/1178630217750876
Kasilo, O. J., Hobane, T., & Nhachi, C. F. B. (1991). Organophosphate poisoning in urban Zimbabwe. Journal of Applied Toxicology, 11(4), 269–272. DOI: https://doi.org/10.1002/jat.2550110407
Kim, J., Shin, S. Do, Jeong, S., Suh, G. J., & Kwak, Y. H. (2017). Effect of prohibiting the use of Paraquat on pesticide-associated mortality. BMC Public Health, 17(1), 1–11. https://doi.org/10.1186/s12889-017-4832-4 DOI: https://doi.org/10.1186/s12889-017-4832-4
Kosamu, I., Kaonga, C., & Utembe, W. (2020). A Critical Review of the Status of Pesticide Exposure Management in Malawi. International journal of environmental research and public health, 17(18), 6727. https://doi.org/10.3390/ijerph17186727 DOI: https://doi.org/10.3390/ijerph17186727
Koulapur, V. V, Pujar, S. S., Honnungar, S. R., Jirli, S. P., & Patil, S. (2015). Epidemiological Profile of Pesticide Poisoning Cases in Bijapur, Karnataka in Southwest India: a Retrospective Study. International Journal of Medical Toxicology and Forensic Medicine, 5 (4), 180–184.
Kuhudzayi, B., & Mattos, D. (2018). A Model for Farmer Support in Zimbabwe-Opportunity for Change. Nebraska Agricultural Economics, 1–5. https://agecon.unl.edu/cornhuskereconomics
Lekei, E., Ngowi, A. V., & London, L. (2017). Acute pesticide poisoning in children: Hospital review in selected hospitals of Tanzania. Journal of Toxicology, 2017. https://doi.org/10.1155/ 2017/4208405 DOI: https://doi.org/10.1155/2017/4208405
Loha, K.M., Lamoree, M., Weiss, J.M., de Boer, J. (2018). Import, disposal, and health impacts of pesticides in the East Africa Rift (EAR) zone: A review on management and policy analysis. Crop Protection, 112, 322-331. https://doi.org/10.1016/j.cropro.2018.06.014. DOI: https://doi.org/10.1016/j.cropro.2018.06.014
Manuweera, G., Eddleston, M., Egodage, S., and Buckley, N. A. (2008). Do targeted bans on insecticides to prevent deaths from self-poisoning result in reduced agricultural output? Environmental Health Perspectives, 116(4), 1–4. DOI:10.1289/ehp.11029 DOI: https://doi.org/10.1289/ehp.11029
Marete, G. M., Lalah, J. O., Mputhia, J., & Wekesa, V. W. (2021). Pesticide usage practices as sources of occupational exposure and health impacts on horticultural farmers in Meru County, Kenya. Heliyon, 7, e06118. https://doi.org/10.1016/j.heliyon.2021.e06118 DOI: https://doi.org/10.1016/j.heliyon.2021.e06118
Maumbe, B. M., & Swinton, S. M. (2003). Hidden health costs of pesticide use in Zimbabwe smallholder cotton growers. Social Science and Medicine, 57(9), 1559–1571. https://doi.org/https://doi.org/10.1016/S0277-9536(03)00016-9 DOI: https://doi.org/10.1016/S0277-9536(03)00016-9
Mergl, R., Koburger, N., Heinrichs, K., Székely, A., Tóth, M. D., et al. (2015). What are the reasons for the large gender differences in the lethality of suicidal acts? An epidemiological analysis in four European countries. PLoS ONE, 10(7), 1–18. https://doi.org/10.1371/journal.pone.0129062 DOI: https://doi.org/10.1371/journal.pone.0129062
Mew, E. J., Padmanathan, P., Konradsen, F., Eddleston, M., Chang, S., et al. (2017). The global burden of fatal self-poisoning with pesticides 2006-15: Systematic review. Journal of Affective Disorders, 219, 93–104. https://doi.org/10.1016/j.jad.2017.05.002 DOI: https://doi.org/10.1016/j.jad.2017.05.002
Mutami, C. (2015). Smallholder Agriculture Production in Zimbabwe: A Survey. Consilience: The Journal of Sustainable Development, 14(2), 140–157. https://doi.org/10.3168/jds.2011-4913 DOI: https://doi.org/10.3168/jds.2011-4913
Navabi, S. M., Navabi, J., Aghaei, A., Shaahmadi, Z., & Heydari, R. (2018). Mortality from Aluminum Phosphide poisoning in Kermanshah Province, Iran: Characteristics and predictive factors. Epidemiology and health, 40, 1–6. https://doi.org/10.4178/ epih.e2018022 DOI: https://doi.org/10.4178/epih.e2018022
Nhari, D. B. (1996). Pesticides in Zimbabwe: toxicity and health implications. In C. F. B. Nhachi & O. M. J. Kasilo (Eds.), Pesticides in Zimbabwe: toxicity and health implications (pp. 38–49). Harare: UZ Publications. Retrieved from https://opendocs.ids.ac.uk/opendocs/handle/20.500.12413/10022
Noghrehchi, F., Dawson, A. H., Raubenheimer, J. E., & Buckley, N. A. (2022). Role of age-sex as underlying risk factors for death in acute pesticide self-poisoning: a prospective cohort study. Clinical Toxicology, 60(2), 184–190. https://doi.org/https://doi.org/ 10.1080/15563650.2021.1921186 DOI: https://doi.org/10.1080/15563650.2021.1921186
Ntzani, E. E., Ntritsos G, C. M., Evangelou, E., & Tzoulaki, I. (2013). Literature review on epidemiological studies linking exposure to pesticides and health effects. European Food Safety Authority Supporting Publications 2013:EN-497, 10(10), 1–159. https://doi.org/10.2903/sp.efsa.2013.en-497 DOI: https://doi.org/10.2903/sp.efsa.2013.EN-497
Oesterlund, A. H., Thomsen, J. F., Sekimpi, D. K., Maziina, J., Racheal, A., and Jørs, E. (2014). Pesticide knowledge, practice and attitude and how it affects the health of small-scale farmers in Uganda: A cross-sectional study. African Health Sciences, 14(2), 420–433. https://doi.org/10.4314/ahs.v14i2.19 DOI: https://doi.org/10.4314/ahs.v14i2.19
Pathak, V. M., Verma, V. K., Rawat, B. S., Kaur, B., Babu, N., et al. (2022). Current status of pesticide effects on the environment, human health and its eco-friendly management as bioremediation: A comprehensive review. Frontiers in Microbiology, 13, 1–29. https://doi.org/10.3389/fmicb.2022.962619 DOI: https://doi.org/10.3389/fmicb.2022.962619
Pedersen, B., Ssemugabo, C., Nabankema, V., & Jørs, E. (2017). Characteristics of pesticide poisoning in rural and urban settings in Uganda. Environmental Health Insights, 11, 1–8. https://doi.org/10.1177/1178630217713015 DOI: https://doi.org/10.1177/1178630217713015
Rao, C. S., Venkateswarlu, V., Surender, T., Eddleston, M., & Buckley, N. A. (2005). Pesticide poisoning in South India: Opportunities for prevention and improved medical management. Tropical Medicine and International Health, 10(6), 581–588. https://doi.org/10.1111/j.1365-3156.2005.01412.x DOI: https://doi.org/10.1111/j.1365-3156.2005.01412.x
Razwiedani, L. L., & Rautenbach, P. G. D. (2017). Epidemiology of organophosphate poisoning in the Tshwane District of South Africa. Environmental Health Insights, 11, 10–13. https://doi.org/ 10.1177/1178630217694149 DOI: https://doi.org/10.1177/1178630217694149
Rotterdam Convention. (2024). Database of Severely Hazardous Pesticide Formulations. Retrieved February 27, 2024, from https://www.pic.int/Procedures/SeverelyHazardousPesticideFormulations/Database/tabid/1369/language/en-US/Default.aspx
Samaria, S., Pandit, V., Akhade, S., Biswal, S., & Kannauje, P. K. (2024). Clinical and epidemiological study of poisoning cases presenting to the emergency department of a tertiary care center in Central India. Cureus, 16(1), 1–13. https://doi.org/10.7759/ cureus.52368 DOI: https://doi.org/10.7759/cureus.52368
Sarkar, M. K., Ghosh, N., Rakesh, U., Prasad, R., & Raj, R. (2022). Acute Aluminium Phosphide poisoning: A case report of rare survival with cardiac, metabolic, hepatic, and renal complications. Journal of Family Medicine and Primary Care, 11(2), 7452–7455. https://doi.org/10.4103/jfmpc.jfmpc_615_22 DOI: https://doi.org/10.4103/jfmpc.jfmpc_615_22
Sekabojja, D., Atuhaire, A., Nabankema, V., Sekimpi, D., Bainomugisa, C., & Jørs, E. (2020). Acute pesticide poisoning case registration in Uganda’s Health Care Facilities. Journal of Environmental and Analytical Toxicology, 10(2), 1–7. https://doi.org/10.4172/2161-0525.10001
Sibani, C., Jessen, K. K., Tekin, B., Nabankema, V., & Jørs, E. (2017). Effects of teaching health care workers on diagnosis and treatment of pesticide poisonings in Uganda. Environmental Health Insights, 11, 1–12. https://doi.org/10.1177/1178630217726778 DOI: https://doi.org/10.1177/1178630217726778
Slabbert, J. A., & Smith, W. P. (2011). Patient transport from rural to tertiary healthcare centres in the Western Cape: Is there room for improvement? African Journal of Emergency Medicine, 1(1), 11–16. https://doi.org/10.1016/j.afjem.2011.04.001 DOI: https://doi.org/10.1016/j.afjem.2011.04.001
Soko, J. J. (2018). Agricultural pesticide use in Malawi. Journal of Health and Pollution, 8(20), 1–7.https://doi.org/10.5696/2156-9614-8.20.181201 DOI: https://doi.org/10.5696/2156-9614-8.20.181201
Ssemugabo, C., Halage, A. A., Neebye, R. M., Nabankema, V., Kasule, M. M., Ssekimpi, D., & Jørs, E. (2017). Prevalence, circumstances, and management of acute pesticide poisoning in hospitals in Kampala City, Uganda. Environmental Health Insights, 11, 1–8. https://doi.org/10.1177/1178630217728924 DOI: https://doi.org/10.1177/1178630217728924
Ssemugabo, C., Nalinya, S., Halage, A. A., Neebye, R. M., Musoke, D., & Jørs, E. (2020). Doctors’ experiences on the quality of care for pesticide poisoning patients in hospitals in Kampala, Uganda: A qualitative exploration using Donabedian’s model. BMC Health Services Research, 20(1), 1–8. https://doi.org/10.1186/s12913-020-4891-6 DOI: https://doi.org/10.1186/s12913-020-4891-6
Tagwireyi, D., Ball, D. E., & Nhachi, C. F. B. (2002). Poisoning in Zimbabwe: A survey of eight major referral hospitals. Journal of Applied Toxicology, 22(2), 99–105. https://doi.org/10.1002/jat.832 DOI: https://doi.org/10.1002/jat.832
Tagwireyi, D., Chingombe, P., Khoza, S., & Maredza, M. (2016). Pattern and epidemiology of poisoning in the East African Region : A literature review. Journal of Toxicology, 2016, 1–26. http://dx.doi.org/10.1155/2016/8789624 Review DOI: https://doi.org/10.1155/2016/8789624
Tajai, P., & Kornjirakasemsan, A. (2023). Predicting mortality in paraquat poisoning through clinical findings, with a focus on pulmonary and cardiovascular system disorders. Journal of Pharmaceutical Policy and Practice, 16(1), 1–9. https://doi.org/10.1186/s40545-023-00635-z DOI: https://doi.org/10.1186/s40545-023-00635-z
Ter Horst, M., Edmund, J. C., & Van der Valk, H. (2023). Risk reduction of highly hazardous pesticides in Ghana. Wageningen, Wageningen Environmental Research, Report 3318. https://doi.org/https://doi.org/10.18174/644354 DOI: https://doi.org/10.18174/644354
Tessema, R. A., Nagy, K., & Ádám, B. (2022). Occupational and environmental pesticide exposure and associated health risks among pesticide applicators and non-applicator residents in rural Ethiopia. Frontiers in Public Health, 10, 01–18. https://doi.org/10.3389/fpubh.2022.1017189 DOI: https://doi.org/10.3389/fpubh.2022.1017189
Teym, A., Melese, M., Fenta, E., Ayenew, T., Fentahun, F., Tegegne, E., & Alamneh, A. A. (2024). Patterns, clinical outcome, and factors associated with poisoning outcomes among poisoned patients in Northwest Ethiopia. SAGE Open Nursing, 10, 1–9. https://doi.org/10.1177/23779608231226081 DOI: https://doi.org/10.1177/23779608231226081
Tudi, M., Ruan, H. D., Wang, L., Lyu, J., Sadler, R., et al. (2021). Agriculture development, pesticide application and its impact on the environment. International Journal of Environmental Research and Public Health, 18(1112), 1–23. https://doi.org/https://doi.org/ 10.3390/ ijerph18031112 Received: DOI: https://doi.org/10.3390/ijerph18031112
Waktola, L. G., Melese, E. B., Mesfin, N., Altaye, K. D., & Legese, G. L. (2023). Prevalence of unfavorable outcome in acute poisoning and associated factors at the University of Gondar comprehensive specialized hospital, Gondar, Northwest Ethiopia: a hospital-based cross-sectional study. Frontiers in public health, 11, 1160182. https://doi.org/10.3389/fpubh.2023.1160182 DOI: https://doi.org/10.3389/fpubh.2023.1160182
World Health Organisation. (2022). Suicide. Retrieved February 28, 2024, fromhttps://www.who.int/news-room/fact-sheets/detail/suicide
World Health Organization. (2020). The WHO Recommended Classification of Pesticides by Hazard and Guidelines to Classification. https://www.who.int/publications-detail-redirect/ 9789240005662
Yatendra, S., Subhash, J. C., Vivekanand, S., & Abhisek, G. (2014). Acute aluminium phosphide poisoning, what is new? The Egyptian Journal of Internal Medicine, 26(3), 99–103. https://doi.org/10.4103/1110-7782.145298 DOI: https://doi.org/10.4103/1110-7782.145298
Zimba, M., & Zimudzi, C. (2016). Pesticide management practices among rural market gardening farmers near Harare, Zimbabwe. South African Journal of Science, 112(9–10), 1–5. https://doi.org/10.17159/sajs.2016/20150443 DOI: https://doi.org/10.17159/sajs.2016/20150443
Zinyemba, C., Archer, E., & Rother, H. A. (2021). Climate change, pesticides and health: Considering the risks and opportunities of adaptation for Zimbabwean smallholder cotton growers. International Journal of Environmental Research and Public Health, 18(1), 1–11. https://doi.org/10.3390/ijerph18010121 DOI: https://doi.org/10.3390/ijerph18010121
Downloads
Published
How to Cite
License
Copyright (c) 2024 Journal of Experimental Biology and Agricultural Sciences

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.